Could vaccines be a cure for antibiotic-resistant bacteria?
Israeli scientists announce 100% effectiveness of mRNA vaccine against Black Plague-causing bacteria in preclinical trial performed on mice.
Bacteria resistant to antibiotics are one of the biggest challenges facing modern medicine.
An estimate published last year by the Lancet found that more than a million deaths could be directly attributed to antimicrobial resistance (AMR) in 2019. In addition, another 3.65 million deaths involved people with diseases that showed some form of AMR.
When those numbers are combined, it makes AMR the third leading cause of death worldwide. And scientists have predicted that by 2050, AMR will kill more people than cancer.
According to Pfizer’s chief scientific officer, one solution could be developing a vaccine strategy for preventing rather than treating these AMR diseases.
“If you get rid of the diseases, then you are not going to have to use as many antibiotics,” said Annaliesa Anderson, senior vice president and chief scientific officer for Pfizer Vaccine Research and Development.
Several vaccines against bacteria have been developed, such as those against tetanus, pertussis (whooping cough) and diphtheria. However, bacteria are much more complex organisms than viruses, and therefore developing vaccines against bacterial infections has taken longer and proved more complex and challenging.
The world's first mRNA vaccine for bacteria?
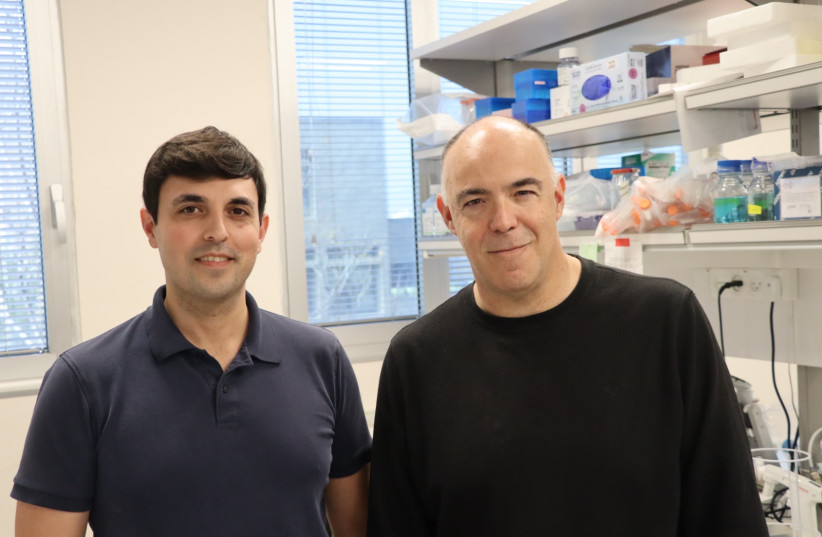
Last week, scientists from Tel Aviv University and the Israel Institute for Biological Research (IIBR) announced that they had developed what could become the world’s first mRNA vaccine for bacteria. When tested on mice, it was found to be 100% effective against yersinia pestis, the bacteria that led to the deadly Black Plague from 1347 to 1351.
The results of their work were published in the peer-reviewed journal Science Advances.
The vaccine was developed and worked similarly to the mRNA vaccine developed by Pfizer and BioNTech. The researchers said it could enable the rapid development of effective vaccines for bacterial diseases when they strike and spread.
"So far, mRNA vaccines, such as the COVID-19 vaccines familiar to all of us, were assumed to be effective against viruses but not against bacteria," explained TAU's Dr. Edo Kon. "The great advantage of these vaccines, in addition to their effectiveness, is the ability to develop them very quickly. Once the genetic sequence of the virus SARS-CoV2 - COVID-19 - was published, it took only 63 days to begin the first clinical trial. However, until now, scientists believed mRNA vaccines against bacteria were biologically undoable."
CORONAVIRUS WAS NAMED for “corona,” a crown, and referred to the spike protein surrounding the antigen. The mRNA coronavirus vaccines work by making antibodies to that spike protein, stopping the virus from infecting the cells and causing disease.
“We made the messenger RNA that can encode that spike protein,” Anderson said, “We mixed it with the nanoparticles, which forms the vaccine. The vaccine is then given to a person, and the nanoparticles help the mRNA enter the person’s cells.”
Once the mRNA has entered the person’s cells, it uses the cell’s machinery to express the protein antigen – the spike protein, in this case. But rather than a live virus coming out of the cells to interact with the immune system, just the spike protein, which has no viral parts, is expressed. It enters the body, comes in contact with the immune system, and makes antibodies, protecting individuals if they come into contact with the pathogen.
Bacteria, however, are a different story. They do not need human cells to produce their proteins, and the proteins produced in bacteria can be different from those made in human cells, even when based on the same genetic sequence, Kon explained.
“Researchers have tried to synthesize bacterial proteins in human cells, but exposure to these proteins resulted in low antibodies and a general lack of protective immune effect in our bodies,” Kon said. “This is because, even though the proteins produced in the bacteria are essentially identical to those synthesized in the lab, being based on the same ‘manufacturing instructions,’ those produced in human cells undergo significant changes, like the addition of sugars, when secreted from the human cell.
“To address this problem, we developed methods to secrete the bacterial proteins while bypassing the classical secretion pathways, which are problematic for this application,” he continued. “The result was a significant immune response, with the immune system identifying the proteins in the vaccine as immunogenic bacterial proteins. To enhance the bacterial protein’s stability and make sure that it does not disintegrate too quickly inside the body, we buttressed it with a section of human protein.”
THE COMBINATION of these two strategies is what led to the whole immune response. Within a week of exposure to the bacteria, all unvaccinated animals died, while those vaccinated with the Israeli vaccine candidate remained alive and well.
Israeli research is 'stellar, opens up possibilities'
Prof. Dan Peer, vice president of research and development and the head of the Laboratory of Precision Nano-Medicine at the Shmunis School of Biomedicine and Cancer Research at TAU, has been working with mRNA for around 20 years. Peer developed a lipids delivery system licensed to BioNTech years before Pfizer began working with the company to create its COVID-19 vaccine.
He said that “as a proof of concept,” the work is “stellar” and opens up several possibilities. First, they are expanding the field of mRNA vaccines for infectious diseases so that they can be used not only for viruses but theoretically for bacteria. They are second, expanding the world’s arsenal against AMR. Third, this breakthrough could lead to others, such as discovering how mRNA could be used to tackle other challenges, such as fungal infections.
Peer said he and his team have been working on this discovery for three-and-a-half years and admit it is still in its infancy. However, he said that after the results of this recent experience, “we believe this is doable.
"Due to excessive use of antibiotics over the last few decades, many bacteria have developed resistance to antibiotics, reducing the effectiveness of these important drugs. Consequently, antibiotic-resistant bacteria already pose a real threat to human health worldwide. Developing a new type of vaccine may provide an answer to this global problem," Peer continued. "Imagine you go to a hospital, and before you are hospitalized, you get a vaccine against certain strains known to be occupied in the hospital, and you are protected."
Pfizer has been developing vaccines that helped prevent antimicrobial resistance for decades, such as its vaccine for preventing invasive disease and pneumonia caused by dozens of streptococcus pneumoniae bacteria that spread by airborne droplets or by direct contact with infected saliva or mucus. These bacteria can lead to severe infections and, in some cases, even death.
However, Anderson said the company’s conjugate vaccine against pneumococcal diseases “is the most complex biological product ever made.”
Three factors for developing a vaccine
ACCORDING TO Kena Swanson, vice president for viral vaccines in Pfizer’s Research & Development department, three factors need to be understood when developing a new vaccine.“We are always trying to understand No. 1 the medical need, and No. 2 is a technical path forward. So, understanding the science, and for some of those diseases with antimicrobial resistance, understanding the right antigens representing that pathogen might elicit a protective immune response. No. 3 is understanding the best way to present these antigens to the immune system,” she said.In the case of SARS-CoV-2, scientists could characterize the antigen so that they could faithfully reproduce them in a way that they were presented naturally on the virus. However, doing this can be more challenging with bacterial protein antigens, Swanson said.
“We have a lot of understanding, but there is still more to be done,” she added, highlighting that there has been only one Phase I clinical trial for chlamydia, for example. In part, this is because the disease was genetically intractable for decades. As a result, it was only in the last 10 years that scientists have been able to tease out what genes are essential and critical for infection versus not to help further guide vaccine design.
“Even the thought of using mRNA as a molecule in a vaccine was not something that happened immediately. Instead, this process took thousands of scientists over many years to understand the mRNA piece, the lipid nanoparticle piece, and the antigen design piece,” Swanson stressed.
“These three important discoveries happened to be present at the right time when that virus emerged,” she added. “Difficult things take incremental discoveries over time that you hope will lead to that big ‘aha moment’ and something successful. That worked for COVID. With some of these other diseases and antimicrobial resistance, we need more time to have that understanding.”
On this note, Peer agreed: “We have a very valid proof of understanding,” he said. “Now we have to choose the right bacteria.”
Jerusalem Post Store
`; document.getElementById("linkPremium").innerHTML = cont; var divWithLink = document.getElementById("premium-link"); if (divWithLink !== null && divWithLink !== 'undefined') { divWithLink.style.border = "solid 1px #cb0f3e"; divWithLink.style.textAlign = "center"; divWithLink.style.marginBottom = "15px"; divWithLink.style.marginTop = "15px"; divWithLink.style.width = "100%"; divWithLink.style.backgroundColor = "#122952"; divWithLink.style.color = "#ffffff"; divWithLink.style.lineHeight = "1.5"; } } (function (v, i) { });