Israel’s first-ever brain cooling at Jerusalem hospital saves life of Filipina nursing assistant

Until now, these patients have been treated with drugs or operated on.
The life of a 46-year-old woman from the Philippines has been saved by the first in-Israel treatment by cooling her brain cells for over a week at Jerusalem’s Shaare Zedek Medical Center (SZMC).
A 46-year-old woman named Norila was rushed to SZMC unconscious and suffering from a life-threatening cerebral hemorrhage. After multidisciplinary and life-saving treatment that included cerebral catheterization, brain surgery and a unique treatment performed for the first time at Shaare Zedek in Israel, her life was saved.
Norila underwent a groundbreaking method for cooling brain cells, which is currently being researched in various parts of the world. Studies show that this technique to prevent strokes in 20-50% of the relevant patients at risk can prevent death in half. This is because it preserves brain cells and brings a better outcome in patients with low survival rates. Patients who are at an 80% to 100% risk of death will have a renewed chance to live with a good neurological outcome, the doctors said.
This first treatment of its kind here was performed by Dr. Stephan Mausbach of the hospital’s neurological intensive care unit – the only one of its kind in Israel. His experience includes working for a decade in bringing leading units in Germany.
Norila, the first patient in Israel to undergo the cooling treatment, came to Israel about 20 years ago to support her family, working as a nursing assistant and raising her daughter, who is now 17. But then her health suddenly deteriorated. After several days during which she suffered from persistent headaches that she shrugged off, she collapsed and was taken by ambulance to the hospital’s emergency medicine. There she underwent a comprehensive series of tests by a multidisciplinary team of the neurology department headed by Dr. Roni Eichel, the neurosurgery department headed by Dr. Nevo Margalit, and Dr. Yaakov Amsalem of the interventional neuroradiology department.
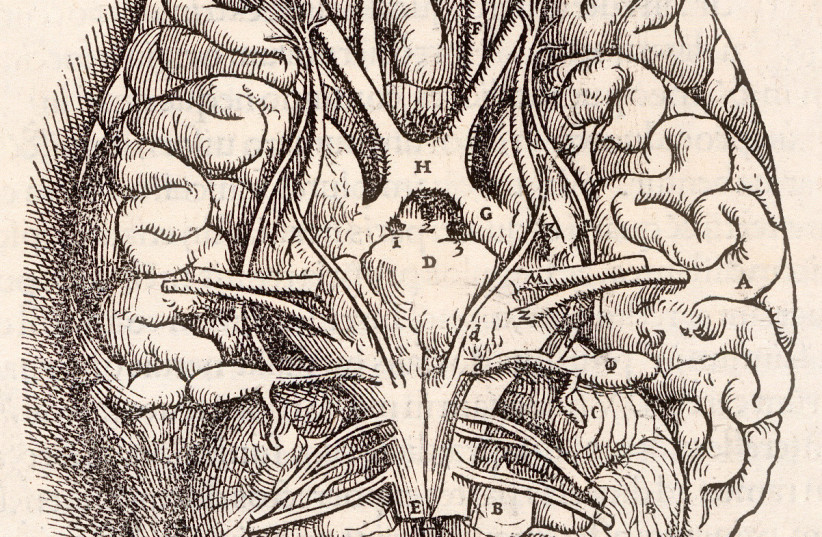
Norila had suffered a spontaneous cerebral aneurysm with a subarachnoid hemorrhage – bleeding in the space that surrounds the brain. Most often, it occurs when a weak area in a blood vessel (aneurysm) on the surface of the brain bursts and leaks. The blood then builds up around the brain and inside the skull increasing pressure there.
While lying in the intensive care unit, she had a cortical cerebral infarction, and a few days later a process of vasospasm. The drug treatment did not help due to increased intracranial pressure and fluid accumulation.
Due to the rapid worsening, an urgent brain catheterization was performed and then surgery to open the skull to lower the intracranial pressure, but to the team’s dismay, these did not lead to improvement, Mausbach said.
The critical cerebral hemorrhage with which Norila was diagnosed had blood flow from the highest that exists under maximal treatment without improvement and at a high risk of death.
After a multidisciplinary consultation of brain system experts in search of the solution that would save her, a therapeutic solution was found that is currently being carried out in a research framework in several German hospitals. Brain cooling is usually performed after resuscitation, but it had not been used as a life-saving treatment in cases of cerebral hemorrhage and life-threatening intracranial pressure, Mausbach continued.
What this could mean for future patients
Until now, these patients have been treated with drugs or operated on. As part of a study in Germany that is currently taking place in 70% of hospitals, cooling is used as a life-saving treatment in cases of excessive bleeding in the patient’s brain. Some of the leading neurology and neurosurgery departments there take patients with a subarachnoid hemorrhage of the highest degree with an 80% to 100% risk of death. Under cooling, they can be given a chance to live with a good neurological outcome in half of the cases.
They performed the cooling using one of the most advanced systems available today that was manufactured by the Arctic Sun company. With this method, they cooled the brain to a temperature of 33 degrees Celsius for eight to 10 days. During this period, the patient remained under the close supervision and monitoring of the medical staff and nurses in the ward led by Ira Gottlieb.
The team monitored the blood flow and the brain cells, we saw that within a few hours, the pressure decreased and the bleeding decreased significantly. During the entire eight days, they held a meeting of a multidisciplinary team that includes neurosurgeons, neurologists and zymologists.
After a significant improvement, they began the warming process, and after a short hospitalization and follow-up, she was discharged to continue a long course of rehabilitation elsewhere and then returned to SZMC to close the skull and complete the complex treatment. “We are very happy and proud of the result. The comprehensive treatment paid off and Norila's life was saved thanks to the innovative treatment,” concluded Mausbach.
Jerusalem Post Store
`; document.getElementById("linkPremium").innerHTML = cont; var divWithLink = document.getElementById("premium-link"); if (divWithLink !== null && divWithLink !== 'undefined') { divWithLink.style.border = "solid 1px #cb0f3e"; divWithLink.style.textAlign = "center"; divWithLink.style.marginBottom = "15px"; divWithLink.style.marginTop = "15px"; divWithLink.style.width = "100%"; divWithLink.style.backgroundColor = "#122952"; divWithLink.style.color = "#ffffff"; divWithLink.style.lineHeight = "1.5"; } } (function (v, i) { });