Technion team discovers important adaptive strategy of the microbiome, impacting immune system
The study focused on species of the Bacteroidales order, some of the most abundant species in the human gut microbiome.
The bacteria in the gut – known as the microbiome – have in recent years emerged as a focal point of scientific exploration, with their intricate roles in our metabolism, nutrition, and overall health coming into sharp focus.
Researchers at the Technion-Israel Institute of Technology in Haifa have now made a discovery that could lead to a better understanding of and treatment for inflammatory bowel diseases (IBD) such as colitis and Crohn’s disease.
Over millions of years of co-evolution with humans, gut bacteria have become indispensable for our immune system’s proper functioning. The gut is a constantly changing organ, undergoing structural, chemical, and mechanical changes and having to adapt to this dynamic environment.
A major mechanism that makes possible such a dynamic adaptation is their ability to undergo rapid genomic changes due to a trait known as plasticity. It has been investigated for years by Professor Naama Geva-Zatorsky and her team in the Technion’s Ruth and Bruce Rappaport Faculty of Medicine and their collaborators. It has just been published in the journal Cell Host and Microbe under the title “Inflammation and bacteriophages affect DNA inversion states and functionality of the gut microbiota.”
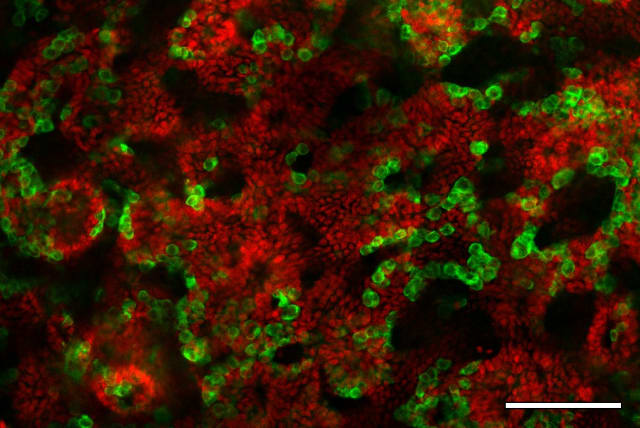
The study focused on species of the Bacteroidales order, some of the most abundant species in the human gut microbiome. While analyzing more than 2,000 healthy and sick people and conducting preclinical research in mice models, the Technion scientists identified distinct patterns of DNA inversions in health and disease. These reversible DNA inversions flip the orientation of main gene segments, switching ON and OFF production of molecules. Interestingly, in Bacteroides fragilis, DNA inversions turned OFF the production of polysaccharide A, a molecule coating the bacteria that beneficially induces regulatory T cells – a specialized immune cell type that suppresses excessive inflammation and maintains gut homeostasis.
The likely culprit is bacteriophages – viruses that infect bacteria. Further examination of fecal samples from IBD patients revealed a striking pattern: the PSA promoter was predominantly in the OFF state, correlating with increased levels of B. fragilis-associated bacteriophages. Subsequent experiments with germ-free mice, colonized with B. fragilis in the presence of bacteriophages, highlighted a significant increase in B. fragilis with the OFF state and a notable reduction in populations of Treg cells.
How this discovery impacts inflammation or viral attacks
Amazingly, the findings revealed an ingenious adaptation strategy used by gut microbes that allows them to dynamically reprogram gene expression based on local conditions like inflammation or viral attacks. However, this biological shape-shifting may worsen disease by crippling production of molecules like PSA that regulate the immune system and reduce gut inflammation.
“This research offers a critical insight into the intricate interactions between gut bacteria and the immune system in inflammatory bowel disease. Our explanation is that the same genomic flexibility that was developed through evolution provides the bacteria with functional plasticity, thereby helping them to adapt to intestinal disease,” commented Geva-Zatorsky. “It opens doors for targeted interventions aimed at restoring the balance of gut microbiota in IBD patients.”
Jerusalem Post Store
`; document.getElementById("linkPremium").innerHTML = cont; var divWithLink = document.getElementById("premium-link"); if (divWithLink !== null && divWithLink !== 'undefined') { divWithLink.style.border = "solid 1px #cb0f3e"; divWithLink.style.textAlign = "center"; divWithLink.style.marginBottom = "15px"; divWithLink.style.marginTop = "15px"; divWithLink.style.width = "100%"; divWithLink.style.backgroundColor = "#122952"; divWithLink.style.color = "#ffffff"; divWithLink.style.lineHeight = "1.5"; } } (function (v, i) { });