This type of cancer is preventable. There's no reason to die from it today

Prof. Tali Levy, director of the gynecology and oncology unit at Wolfson Hospital, explains everything you need to know about cervical cancer, and how risk can be lowered from a young age.
Prof. Tali Levy recalls a busy clinic day as usual, with many women waiting to be examined. The women talk to each other and everyone is a bit stressed since there are inevitable delays.
One patient is Einat (pseudonym), a 38-year-old mom of three children, the youngest of whom is three years old. At the exam, Einat explains that she's had irregular vaginal bleeding for about four months and bleeding during intercourse. Recently, the bleeding has intensified and she has pain in her lower abdomen.
Einat looks scared, a little pale. Levy tries to calm her down and asks if she's had a recent gynecological exam. It turns out that Einat hasn't been examined or had diagnostic tests since the birth of her youngest.
Also, she's not sure if she's ever had a Pap smear, the main test which detects cervical cancer. Levy prepares Einat for the exam. As soon as she inserts a speculum, the plastic device used to see the vagina and cervix, her heart drops. In the cervix is a lump about 5 centimeters in size which is protruding and bleeding. It's absolutely clear that Einat has a cancerous tumor in the cervix.
The thoughts swirl in Levy's head. How can she tell this young mom with small kids that this lump is causing the bleeding? Sadness overwhelms the doctor. Could it have been possible to detect the beginning of the cancer's development at an earlier stage via periodic exams? Could this cancer have been prevented by vaccination against the human papillomavirus, known as HPV?
Levy tells Einat what she sees and explains that a cervical biopsy and additional tests are required to assess the tumor's margins and which stage the cancer is. Einat definitely has cervical cancer which has metastasized (spread) to the lymph nodes and pelvis. She needs radiation treatment and chemotherapy, and only time will tell if she'll recover and get to raise her children.
What are the risk factors behind cervical cancer?
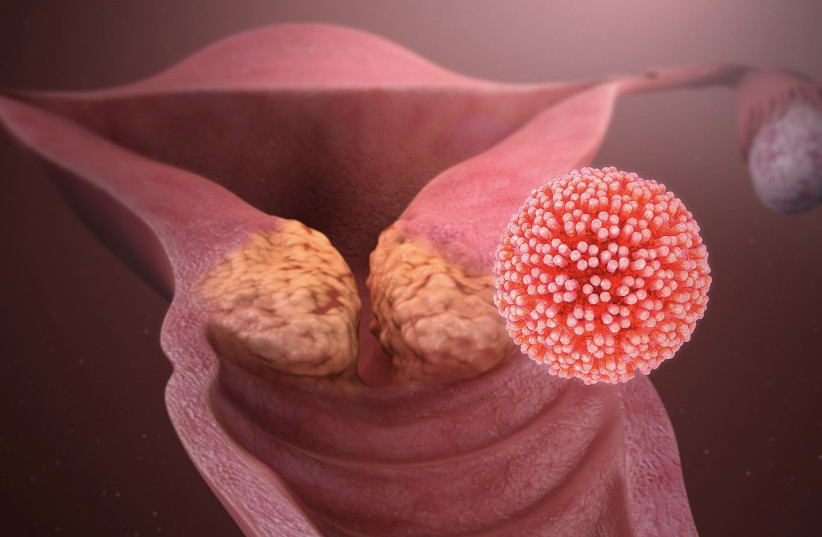
Cervical cancer is a malignancy caused by infection with the human papillomavirus (HPV). This virus is considered the most common contaminant transmitted by sexual contact in the world, and the main cause of precancerous changes, cervical cancer and conical viral warts, condylomata, in the genitals. The main infection is through any kind of intercourse.
HPV has over 150 known strains. About 20 of them are related to the development of premalignant changes and cervical cancer, as well as malignancies in the mouth and throat area when infection is through oral sex. Two main HPV strains, 16 and 18, are responsible for about 70% of cervical cancer cases. Strains 6 and 11 cause about 90% of genital warts, i.e. condylomata, as well as low-grade premalignant lesions.
Most women and men become infected with HPV in the first few years of having sex. It's important to know that the high infection rates in women and men are the same. HPV infection has no symptoms and the body's natural defense system overcomes it naturally, usually within a year or two. Since the virus is very common in the population, the cumulative chance of a woman contracting the virus is about 80%.
In a small percentage of infected women, the virus stays in the body and remains permanently in the cervical cells. Perpetual infection with HPV happens especially if you get infected with HPV strains that can cause the development of precancerous changes and cervical cancer and not with strains that cause warts.
Smoking and taking birth control pills are additional risk factors for the development of malignancy in the cervix with constant virus infection.About 90% of all infections are latent, or hidden. Even when pre-cancerous changes have already developed, most of the time, there aren't any symptoms. So, it's crucial to perform screening and diagnostic tests for cervical cancer.
Get Pap tests and the vaccine
The Pap test and the HPV test allow early detection of premalignant changes which significantly reduce the development of cervical cancer and mortality from it. The global recommendation is to test from age 25, once every 3 years. The cessation of screening tests for cervical cancer is recommended between ages 65-70 if three previous Pap tests were normal.
Cervical cancer is a cancer that can be detected early and prevented so there's great importance in raising awareness of screening tests and therapeutic options in the premalignant stages. There's an effective vaccine against nine types of papilloma: 6 and 11 which cause about 90% of genital warts,16 and 18 which cause about 70% of cervical cancer cases, and the vaccine can provide protection from another five more virulent strains.
Ideally, girls should be vaccinated before their first sexual experience, since most people become infected with HPV within the first three years of having sex. Global studies show that among girls and young women who've been vaccinated, there's a significant reduction in the development of pre-cancerous and even cancerous changes in the cervix.
The HPV vaccine is given in eighth grade for girls and boys and is approved for women and men up to age 45.
Health organizations emphasize that it's important that women who've been vaccinated continue to undergo screening tests for the early detection of precancerous cervical changes to prevent the development of cancer.
Cervical cancer is a preventable cancer. Vaccinate your kids and get checked regularly. There's no reason that in the 21st century, women will still get diagnosed with advanced-stage cervical cancer or die from this disease.
Jerusalem Post Store
`; document.getElementById("linkPremium").innerHTML = cont; var divWithLink = document.getElementById("premium-link"); if (divWithLink !== null && divWithLink !== 'undefined') { divWithLink.style.border = "solid 1px #cb0f3e"; divWithLink.style.textAlign = "center"; divWithLink.style.marginBottom = "15px"; divWithLink.style.marginTop = "15px"; divWithLink.style.width = "100%"; divWithLink.style.backgroundColor = "#122952"; divWithLink.style.color = "#ffffff"; divWithLink.style.lineHeight = "1.5"; } } (function (v, i) { });